Introduction
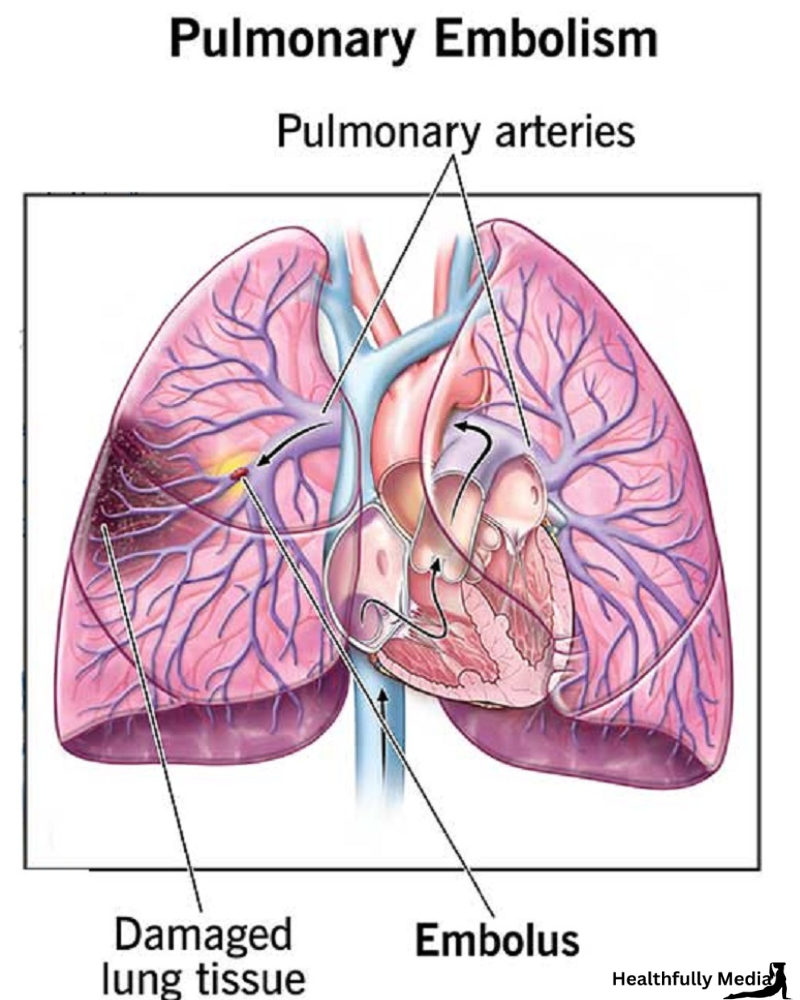
Pulmonary embolism (PE) is a life-threatening medical condition that occurs when a blood clot travels to the lungs, blocking one or more pulmonary arteries. This article delves into the intricacies of pulmonary embolism, exploring its causes, symptoms, and various treatment options.
What Is Pulmonary Embolism (PE)?
Pulmonary embolism, often referred to as PE, is a serious medical condition characterized by the sudden blockage of one or more pulmonary arteries in the lungs. Typically, this blockage occurs when a blood clot, usually originating in the legs or other parts of the body, breaks free and travels through the bloodstream, eventually reaching the lungs. This condition can be life-threatening and requires immediate medical attention.
Causes of Pulmonary Embolism
Understanding the causes of pulmonary embolism is crucial for prevention and early detection. Several factors can contribute to the development of blood clots that lead to PE:
1. Deep Vein Thrombosis (DVT)
One of the primary causes of pulmonary embolism is deep vein thrombosis (DVT). DVT occurs when blood clots form in the deep veins of the legs or pelvis. These clots can dislodge and travel to the lungs, causing a PE.
2. Prolonged Immobility
Situations that involve prolonged immobility, such as long-haul flights or bed rest after surgery, can increase the risk of blood clot formation and, consequently, pulmonary embolism.
3. Surgery and Trauma
Patients undergoing major surgeries or those who have experienced traumatic injuries are at a higher risk of developing blood clots, which can lead to PE.
4. Smoking
Smoking damages blood vessels and increases the risk of blood clot formation, making it a significant risk factor for pulmonary embolism.
Recognizing the Symptoms
Detecting pulmonary embolism early is critical for prompt treatment. Recognizing the common symptoms can help individuals seek medical attention in a timely manner:
1. Shortness of Breath
One of the hallmark symptoms of PE is sudden, unexplained shortness of breath. This may be accompanied by chest pain and a rapid heart rate.
2. Chest Pain
Chest pain, especially when breathing deeply or coughing, is a common symptom of PE. It can range from mild discomfort to severe pain.
3. Coughing and Hemoptysis
Some individuals with PE experience coughing, often with bloody sputum, a condition known as hemoptysis.
Diagnosing Pulmonary Embolism
Diagnosing PE involves a combination of clinical evaluation and medical tests. Common diagnostic methods include:
1. Computed Tomography (CT) Pulmonary Angiography
CT pulmonary angiography is a key diagnostic tool that allows physicians to visualize blood clots in the pulmonary arteries.
2. Blood Tests
Blood tests can help identify certain markers that indicate the presence of a blood clot.
Treatment Options
Timely and appropriate treatment is essential to prevent complications and improve outcomes for individuals with pulmonary embolism. Treatment options include:
1. Anticoagulant Medications
Anticoagulant medications, such as heparin and warfarin, are commonly prescribed to prevent further blood clot formation.
2. Thrombolytic Therapy
In severe cases of PE, thrombolytic therapy may be administered to dissolve the clot quickly.
3. Surgical Intervention
In rare instances, surgical removal of the clot may be necessary, especially when the patient is in critical condition.
Conclusion
Pulmonary embolism is a serious medical condition that demands prompt attention and appropriate treatment. Understanding its causes, recognizing its symptoms, and knowing the available treatment options are essential for both prevention and managing this potentially life-threatening condition.
FAQs
1. Can pulmonary embolism be prevented?
Yes, pulmonary embolism can often be prevented by lifestyle changes, including regular exercise, quitting smoking, and staying hydrated, especially during long flights.
2. What are the long-term effects of pulmonary embolism?
While prompt treatment can significantly reduce the risk of long-term complications, some individuals may experience residual symptoms or complications, such as post-thrombotic syndrome.
3. Are there any risk factors that increase the likelihood of developing PE?
Yes, several risk factors, including a history of DVT, family history of blood clots, and certain medical conditions, can increase the risk of developing pulmonary embolism.
4. Can pulmonary embolism be fatal?
Yes, if not promptly treated, pulmonary embolism can be fatal. It is crucial to seek immediate medical attention if you suspect you have PE.
5. Is there a link between COVID-19 and pulmonary embolism?
Yes, COVID-19 has been associated with an increased risk of blood clots, including pulmonary embolism. Individuals who have had COVID-19 should be aware of this risk and seek medical attention if they experience symptoms of PE