1. Introduction: What is Hypercapnia?
Hypercapnia, also known as carbon dioxide toxicity or hypercarbia, refers to a condition characterized by an abnormally high level of carbon dioxide (CO2) in the blood. Normally, the body eliminates carbon dioxide through respiration. However, when the lungs fail to remove sufficient CO2, it builds up in the bloodstream, leading to hypercapnia. This condition can have adverse effects on various organ systems, particularly the respiratory and nervous systems.
2. Causes of Hypercapnia
There are several potential causes of hypercapnia, including:
2.1. Respiratory Conditions
Respiratory conditions that impair lung function, such as chronic obstructive pulmonary disease (COPD), asthma, pneumonia, and bronchitis, can contribute to hypercapnia. These conditions hinder the exchange of gases, leading to an accumulation of carbon dioxide in the bloodstream.
2.2. Central Nervous System Disorders
Certain central nervous system disorders, like brainstem injury, stroke, or conditions affecting the respiratory centers in the brain, can disrupt the normal breathing process. This disruption can result in inadequate ventilation and subsequent hypercapnia.
2.3. Obesity Hypoventilation Syndrome
Obesity hypoventilation syndrome (OHS) occurs when individuals with obesity experience impaired breathing, leading to decreased ventilation and hypercapnia. The excess weight can put pressure on the chest, limiting the expansion of the lungs and affecting breathing patterns.
2.4. Medications and Anesthesia
Certain medications, such as sedatives and opioids, can depress the respiratory system, reducing the drive to breathe and potentially causing hypercapnia. Additionally, anesthesia during surgery can temporarily disrupt breathing patterns and contribute to increased carbon dioxide levels.
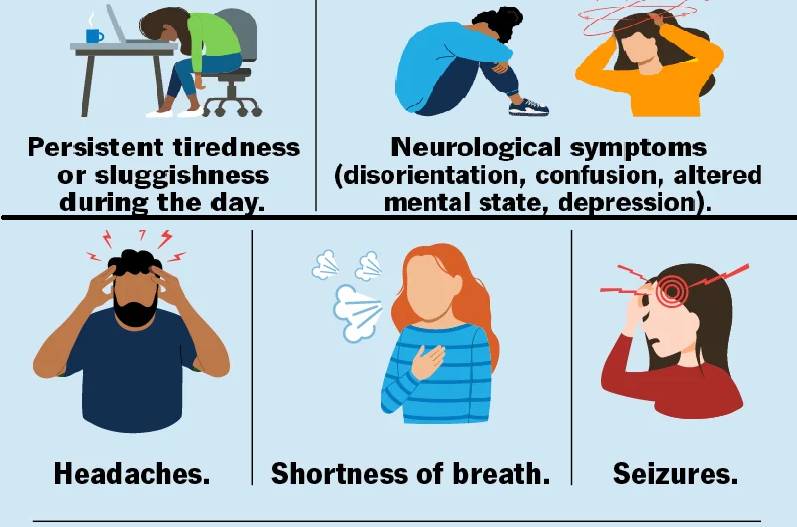
3. Symptoms of Hypercapnia
Hypercapnia can manifest through various symptoms, which may vary depending on the severity of the condition. Common symptoms of hypercapnia include:
- Shortness of breath
- Rapid breathing
- Confusion or cognitive impairment
- Headaches
- Drowsiness or fatigue
- Flushing or redness of the skin
- Tremors or muscle twitches
- Elevated heart rate
- Sweating
- Chest pain
4. Diagnosis of Hypercapnia
To diagnose hypercapnia, healthcare professionals will evaluate the patient’s medical history, conduct a physical examination, and perform specific tests. These tests may include:
- Arterial blood gas (ABG) test: This test measures the levels of oxygen and carbon dioxide in the blood, helping to determine the extent of hypercapnia.
- Pulmonary function tests: These tests assess lung function and can help identify respiratory conditions contributing to hypercapnia.
- Chest X-ray or CT scan: Imaging tests may be used to examine the lungs and identify any abnormalities.
- Sleep studies: In some cases, sleep studies may be conducted to evaluate breathing patterns during sleep and detect conditions like sleep apnea.
5. Treatment Options for Hypercapnia
The treatment of hypercapnia aims to improve lung function, enhance ventilation, and normalize carbon dioxide levels. The specific treatment approach may vary depending on the underlying cause and severity of hypercapnia. Some common treatment options include:
- Oxygen therapy: Supplemental oxygen can help increase oxygen levels in the blood and alleviate symptoms associated with hypercapnia.
- Medications: Bronchodilators, corticosteroids, and other respiratory medications may be prescribed to manage underlying respiratory conditions contributing to hypercapnia.
- Non-invasive ventilation: Devices such as continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP) machines can assist with breathing and improve ventilation.
- Pulmonary rehabilitation: This comprehensive program includes exercise, education, and breathing techniques to enhance lung function and overall respiratory health.
- Surgical interventions: In some cases, surgery may be necessary to address underlying conditions contributing to hypercapnia, such as removing lung tumors or correcting structural abnormalities.
6. Lifestyle Changes to Manage Hypercapnia
In addition to medical interventions, individuals with hypercapnia can make certain lifestyle modifications to manage their condition effectively. These include:
- Quitting smoking: Smoking can further impair lung function and exacerbate hypercapnia. Quitting smoking can significantly improve respiratory health.
- Regular exercise: Engaging in regular physical activity can help strengthen the respiratory muscles and enhance lung capacity.
- Maintaining a healthy weight: For individuals with obesity hypoventilation syndrome, losing weight can alleviate the pressure on the chest and improve breathing patterns.
- Following a balanced diet: Consuming a nutritious diet rich in fruits, vegetables, whole grains, and lean proteins can support overall respiratory health.
- Avoiding respiratory irritants: Minimizing exposure to environmental pollutants, such as dust, chemical fumes, and allergens, can help reduce respiratory symptoms.
7. Prevention of Hypercapnia
While certain causes of hypercapnia may be unavoidable, there are preventive measures individuals can take to reduce the risk of developing this condition. These preventive strategies include:
- Seeking timely treatment for respiratory conditions: Early diagnosis and management of respiratory conditions like COPD or asthma can help prevent the progression to hypercapnia.
- Adhering to prescribed medications: Taking respiratory medications as prescribed by healthcare professionals can help maintain optimal lung function and prevent exacerbations.
- Practicing respiratory hygiene: Following good respiratory hygiene, such as covering the mouth and nose while coughing or sneezing, can minimize the risk of respiratory infections that may contribute to hypercapnia.
8. Conclusion
Hypercapnia is a condition characterized by elevated levels of carbon dioxide in the blood. It can result from various respiratory and central nervous system disorders. Prompt diagnosis and appropriate treatment are essential to manage hypercapnia effectively. Medical interventions, lifestyle modifications, and preventive measures can help individuals lead a better quality of life and minimize the impact of hypercapnia on their overall health.
9. FAQs
Q1. Can hypercapnia be life-threatening? Hypercapnia can become life-threatening if left untreated or if the underlying condition causing it worsens. It is crucial to seek medical attention and follow the prescribed treatment plan.
Q2. Is hypercapnia reversible? In many cases, hypercapnia is reversible with appropriate treatment. Treating the underlying cause and improving lung function can help normalize carbon dioxide levels.
Q3. Can hypercapnia occur during sleep? Yes, hypercapnia can occur during sleep, especially in individuals with sleep apnea or other respiratory disorders. Sleep studies can help diagnose and manage hypercapnia during sleep.
Q4. Can anxiety cause hypercapnia? While anxiety itself may not directly cause hypercapnia, it can lead to rapid breathing or hyperventilation, which can lower carbon dioxide levels in the blood. This can result in respiratory alkalosis but not necessarily hypercapnia.
Q5. Is hypercapnia a common condition? Hypercapnia is more commonly seen in individuals with chronic respiratory conditions like COPD. However, it can occur in other situations as well, depending on the underlying causes